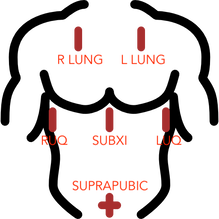
The FAST exam is a tool for identifying the presence of free intra-peritoneal fluid, pleural fluid, and pericardial fluid in trauma patients. The extended FAST, or "e-FAST", also assesses for the presence of pneumothorax.
Utility
It was developed as a way of evaluating hypotensive patients who presented after blunt abdominal trauma or any chest trauma. A hemodynamically unstable trauma patient with a positive FAST goes immediately to the OR for exploratory surgery. As a resident, it may feel like most of your FAST exams are educational because blunt trauma patients are frequently stable enough for CT but that is okay because the exam's utility is closely tied to operator experience. With practice, a well-executed FAST should take no more than 3 to 5 minutes. The FAST is not as useful to evaluate penetrating abdominal injury as this cohort of patients will virtually always get a CT or go directly to the OR for exploratory surgery. When patients arrive to the ED after a penetrating chest wound, the e-FAST allows for quick identification of a hemo/pneumothorax. Also make note that a hole in the chest tells you very little about the projectile's trajectory. Therefore, a patient who just got shot in the back may not only need a chest tube but also an ex-lap for their diaphragm and liver injury! Don't forget the FAST!
The data for performing an ED pericardiocentesis for traumatic cardiac tamponade is less straight forward in unstable patients. If a patient exhibits signs of life for EMS or in the ED and then arrests from their traumatic injuries, ultrasound can aid in determining whether or not to "open the chest". Studies have demonstrated that sonographic cardiac standstill in patients presenting with traumatic arrest from a penetrating chest wound is highly predictable for thoracotomy futility.
Outside the realm of trauma, the FAST exam is a great bedside tool to evaluate for intra-abdominal fluid in other clinical scenarios such as decompensated liver disease and suspected ruptured ectopic pregnancies.
It was developed as a way of evaluating hypotensive patients who presented after blunt abdominal trauma or any chest trauma. A hemodynamically unstable trauma patient with a positive FAST goes immediately to the OR for exploratory surgery. As a resident, it may feel like most of your FAST exams are educational because blunt trauma patients are frequently stable enough for CT but that is okay because the exam's utility is closely tied to operator experience. With practice, a well-executed FAST should take no more than 3 to 5 minutes. The FAST is not as useful to evaluate penetrating abdominal injury as this cohort of patients will virtually always get a CT or go directly to the OR for exploratory surgery. When patients arrive to the ED after a penetrating chest wound, the e-FAST allows for quick identification of a hemo/pneumothorax. Also make note that a hole in the chest tells you very little about the projectile's trajectory. Therefore, a patient who just got shot in the back may not only need a chest tube but also an ex-lap for their diaphragm and liver injury! Don't forget the FAST!
The data for performing an ED pericardiocentesis for traumatic cardiac tamponade is less straight forward in unstable patients. If a patient exhibits signs of life for EMS or in the ED and then arrests from their traumatic injuries, ultrasound can aid in determining whether or not to "open the chest". Studies have demonstrated that sonographic cardiac standstill in patients presenting with traumatic arrest from a penetrating chest wound is highly predictable for thoracotomy futility.
Outside the realm of trauma, the FAST exam is a great bedside tool to evaluate for intra-abdominal fluid in other clinical scenarios such as decompensated liver disease and suspected ruptured ectopic pregnancies.
The Data
- Able to detect as little as 150-200 cc of free intra-peritoneal fluid.
- Able to detect as little as 20 cc of pericardial fluid
- Detection of intra-abdominal injury in ADULT blunt trauma
- Sensitivity (%): 74
- Specificity (%): 96
- LR (POS): 30
- LR (NEG): 0.26
- Detection of intra-abdominal injury in PEDIATRIC blunt trauma
- Sensitivity (%): 35
- Specificity. (%): 96
- LR (POS): 10.8
- LR (NEG): 0.65
- Detection of pneumothorax
- Sensitivity (%): ***
- Specificity (%): ***
- LR (POS): ***
- LR (NEG): ***
Practice pearls: The order in which the e-FAST views are obtained is largely determined by the clinical scenario. If the patient is hemodynamically unstable and PNX or cardiac tamponade are high on the differential, you would begin with the lung and cardiac windows because the presence of a pneumothorax potentiates the immediate need of a chest tube. If a patient is hypotensive after motor vehicle collision, has a seatbelt sign, is oxygenating well, and is complaining of abdominal pain one would look at abdomen first to look for free fluid.
Examples (Normal)
Examples (Positive FAST)
References
- Liang, T., Roseman, E., Gao, M., & Sinert, R. (2019). The Utility of the Focused Assessment With Sonography in Trauma Examination in Pediatric Blunt Abdominal Trauma: A Systematic Review and Meta-Analysis. Pediatric Emergency Care. http://doi.org/10.1097/PEC.0000000000001755
- M Liu, C Lee, K P’Eng. Prospective comparison of diagnostic peritoneal lavage, computed tomographic scanning, and ultrasonography for the diagnosis of blunt abdominal trauma. J Trauma 1995; 39(2):375-380.
- Nishijima DK, Simel DL, Wisner DH, Holmes JF. Does this adult patient have a blunt intra-abdominal injury?. JAMA. 2012;307(14):1517–1527. doi:10.1001/jama.2012.422
- Savatmongkorngul, Sorravit et al. “Focused assessment with sonography for trauma: current perspectives.” Open access emergency medicine : OAEM vol. 9 57-62. 26 Jul. 2017, doi:10.2147/OAEM.S120145